
How Businesses are Leveraging AI and IoT to Build Metaverse Ecosystems
March 24, 2025
How Are AI and L2 Redefining DEX Aggregator Development?
March 24, 2025In psychology, there is a concept known as the “peak-end rule.” This rule suggests that our memories of an experience are heavily influenced by the most intense moment (the peak) and the very end of the experience, rather than the overall duration or average experience. Businesses navigating the world of healthcare offer the best patient support to create a seamless and stress-free experience. However, one critical challenge at the final touchpoint, medical billing, can overshadow even the best medical care offered by the providers.
“According to a report, nearly 80% of medical bills contain errors, highlighting the urgent need for a more reliable and transparent billing system.”
Errors in medical billing can have far-reaching consequences as patients may face unexpected bills, insurers may reject claims, and healthcare providers may experience revenue loss. This is where blockchain technology steps in. Blockchain healthcare solutions offer a transparent, decentralized, and tamper-proof solution to eliminate inaccuracies, prevent fraud, and streamline the billing process. Blockchain medical billing enables healthcare providers to ensure that the final impression they leave is one of trust, efficiency, and reliability. But how can blockchain-based medical billing ensure this? Let’s find out in this blog.
Why Medical Billing is Crucial for a Smooth Healthcare System
Medical billing is a critical component of the healthcare ecosystem. Learn how-
- Financial Lifeline for Healthcare Providers
Medical billing shows that healthcare providers, such as hospitals, clinics, and physicians, are compensated for the services they render. Without accurate and timely billing, healthcare providers may face cash flow issues, which can impact their ability to operate effectively.
- Facilitates Insurance Claims Processing and Verification
Medical billing represents that services provided are properly documented, coded, and billed. It helps verify a patient’s insurance coverage before services are rendered. Additionally, it determines whether the patient is eligible for the services and ensures that the healthcare provider will receive reimbursement from the insurance company.
- Streamlines Revenue Cycle Management
Medical billing is a key part of the revenue cycle management process, which includes patient registration, charge capture, claim submission, payment posting, and denial management. Efficient billing processes help healthcare providers maintain a steady revenue stream and reduce administrative burdens.
- Bridges the Gap Between Providers and Payers
Medical billing acts as a communication tool between healthcare providers and insurance companies. Payers with accurate medical billing will have a clear understanding of the services provided, the costs involved, and the reimbursement process.
The Hidden Vulnerabilities in Medical Billing
Now that you understand the importance of medical billing, it’s equally crucial to recognize its complexity, which should not be understated. The complex medical billing process makes this system vulnerable to several risks.
Below, we have covered some risks associated with medical billing that can lead to errors with far-reaching consequences.
Common Types of Medical Billing Fraud
- Billing for Services Not Rendered: This involves claiming reimbursement for treatments, procedures, or supplies that were never provided to the patient.
- Upcoding: This risk occurs when a provider bills for a more expensive service or procedure than the one actually performed.
- Unbundling: This risk involves breaking down a single, bundled procedure or service into multiple smaller codes to bill for each part separately, thus increasing the overall reimbursement.
- Phantom Billing: It involves billing for services or supplies that never happened or were never provided to the patient.
- Duplicate Billing: It occurs when a provider submits multiple claims for the same service or procedure.
- Falsifying Patient Diagnoses: Some providers falsify patient diagnoses to justify unnecessary procedures or treatments, leading to higher reimbursement.
- Administrative inefficiencies: Human errors, miscommunication, and outdated systems contribute to billing errors.
Blockchain-based Medical Billing- A Powerful Solution
As per Grand View Research, the global market size of blockchain technology in healthcare was valued at approximately USD 7.04 billion in 2023 and is projected to expand at a CAGR of 63.3% between 2024 and 2030.
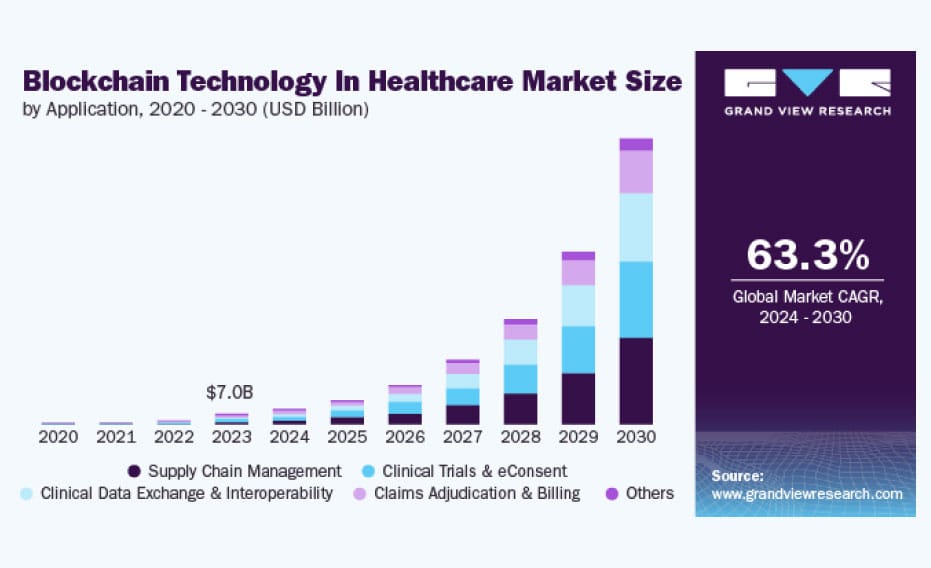
Image Src: Grand View Research
The rising demand for better solutions that can handle sensitive patient information and streamline processes in healthcare administration, such as medical billing and claim processing, has led to the adoption of blockchain in recent years. The numbers are even expected to grow in the coming years as well.
Blockchain is a revolutionary solution that brings transparency, automation, and security into the billing process. It eliminates the system inefficiencies that often become a major reason for claim disputes, delayed payments, and rising administrative costs. Embracing this transformation is crucial, as it brings numerous benefits that enhance the entire billing ecosystem, offering greater transparency, efficiency, and security for insurers, patients, and healthcare providers alike.
Benefits of Leveraging Blockchain for Medical Billing
- Enhanced Data Accuracy and Integrity
One of the primary causes of medical billing errors is inaccurate or incomplete data. Blockchain medical billing can address this issue by providing a single source of truth for all billing-related information. When a patient’s medical record is created or updated, it is stored on the blockchain with a unique patient ID to maintain privacy. The decentralized, tamper-proof ledger ensures that all stakeholders have access to the same accurate and up-to-date information., which eliminates discrepancies caused by outdated or inconsistent data across different systems.
- Automated Billing Processes
Once the patient’s treatment details are recorded on the blockchain, a smart contract is triggered that automates the medical billing process. For example, when a healthcare provider submits a claim, the smart contract can automatically verify the patient’s eligibility, validate the medical codes, and process the payment. It speeds up the billing process and ensures that all transactions are accurate and compliant with regulatory requirements.
- Medical Billing Fraud Detection and Prevention
Fraudulent activities, such as upcoding or unbundling, are significant contributors to medical billing errors and often result from system inefficiencies or human error. Since all records are immutable and stored in a decentralized system, detecting and preventing medical billing fraud becomes easier. All transactions recorded on the blockchain create an auditable trail that authorized parties can review. Any suspicious activity can be quickly identified and addressed.
- Improved Interoperability
The lack of interoperability between healthcare systems is a major barrier to accurate medical billing. Blockchain medical billing can facilitate seamless data exchange between different systems by providing a standardized and secure platform for sharing information. All stakeholders in this decentralized and secure system have access to the same data, which significantly reduces the risk of errors caused by incomplete or inconsistent information.
- Patient Empowerment
Leveraging blockchain for medical billing is a smart move as it provides more control to patients over their medical records and billing information. Patients can access their records on the blockchain, verify the accuracy of their bills, and dispute any discrepancies. It reduces the likelihood of billing errors and enhances patient trust and satisfaction.
Blockchain in Medical Billing: Why You Need an Expert for Integration
A blockchain development company helps maintain efficiency, security, and compliance in medical billing. With expert developers, industry knowledge, and a proven track record, a trusted company delivers solutions tailored to the evolving needs of healthcare providers and insurers.
Why choose a reputable company for blockchain integration in medical billing?
- Domain Expertise & Compliance Assurance
A reputable blockchain healthcare development company understands the complexities of medical billing regulations. Hence, it focuses on building solutions that meet strict compliance standards, safeguard patient data, and enable seamless claim processing.
- Custom-Built & Scalable Solutions
Unlike generic platforms, a blockchain development company builds customized medical billing solutions that integrate effortlessly with existing healthcare systems. With expertise in smart contracts and blockchain programming languages, they deliver a seamless, transparent, and fraud-resistant billing system that improves financial accuracy.
- Seamless Implementation & Ongoing Support
From initial consultation to deployment, a professional blockchain firm ensures smooth implementation with round-the-clock support and maintenance. Their hands-on approach reduces operational risks and maximizes efficiency.
- Proven Trust & Reliability
A top-tier blockchain development company brings a history of successful healthcare implementations. This is what helps them stand out from the crowd when it comes to transforming medical billing with accuracy, transparency, and cost-efficiency.
When looking for an expert to leverage blockchain for medical billing, trust the one who understands both the technology and the industry’s demands.
Conclusion
Medical billing errors are a significant challenge in the healthcare industry, which can lead to financial losses, operational inefficiencies, and patient dissatisfaction. Blockchain has emerged as a revolutionary solution to address these issues as it creates a more transparent, efficient, and patient-centric billing system, where healthcare providers can automate claims processing, reduce fraudulent transactions, and ensure accurate, tamper-proof records. Using blockchain for medical billing enables healthcare organizations to reduce errors, improve trust, and ultimately deliver better care to patients.
Antier transforms the medical billing experience with advanced blockchain solutions. With a team of 700+ experts skilled in top blockchain programming languages like Solidity, Rust, and Hyperledger, Antier helps healthcare providers create secure, automated, and error-free billing systems. We integrate blockchain into existing healthcare setups to ensure seamless claims processing, instant verification, and complete fraud protection. Our commitment to on-time delivery means healthcare organizations can switch to a smarter billing system without any disruptions. Additionally, with 24/7 support, we ensure smooth operations and immediate assistance whenever needed.
Partnering with us for blockchain healthcare development services would be a strategic move toward building a secure, transparent, and efficient medical billing system. Connect with us today!



